Associating herpes zoster ophthalmicus with cerebral vasculitis
Herpes zoster ophthalmicus is associated with vasculopathy and cerebral infarction and has significant morbidity and mortality when untreated
10/07/2023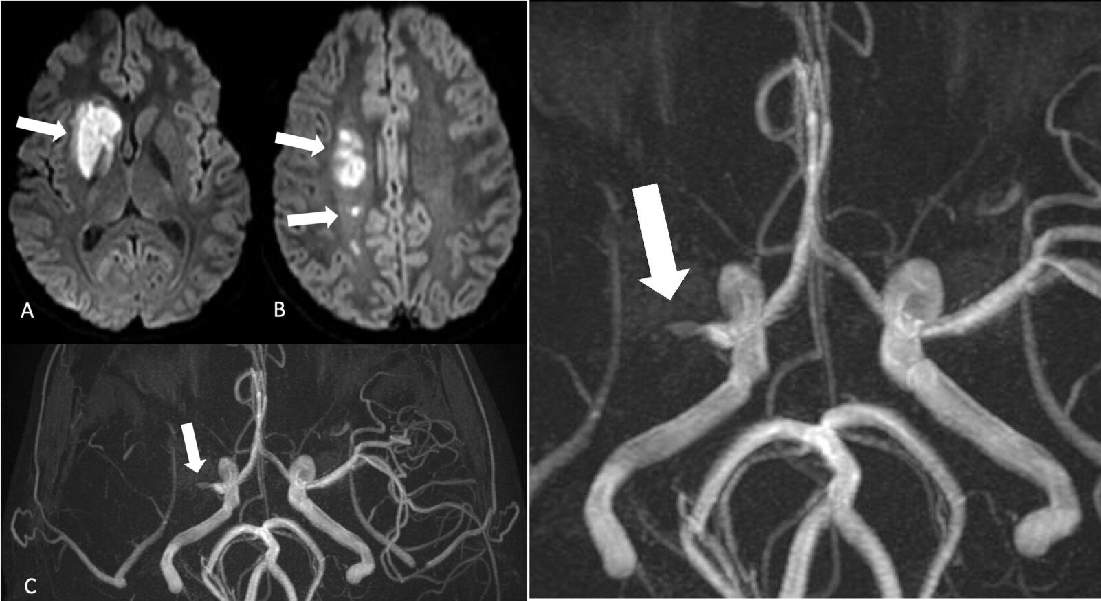
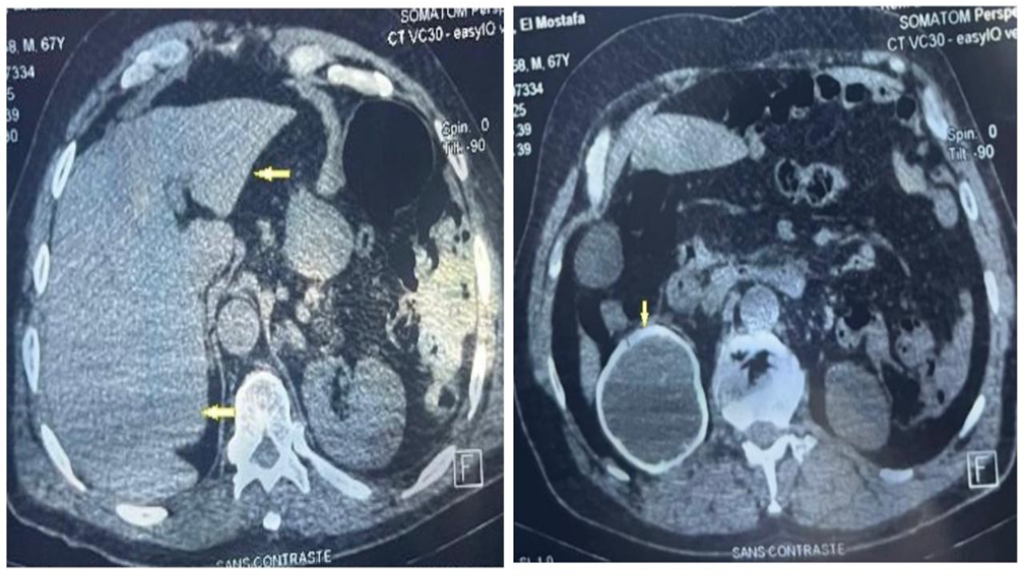
Axial diffusion-weighted images (DWI) showing right basal ganglia, internal capsule, and deep white matter hyperintensity (arrows), which had corresponding hypointensity on the apparent diffusion coefficient (ADC) map (not shown)
Paiva JLR et al. – Herpes zoster ophthalmicus and cerebral vasculitis
Jean Levi Ribeiro de Paiva[1], Tânia Aparecida Marchiori de Oliveira Cardoso[2] and Fabiano Reis[1]
[1]. Universidade Estadual de Campinas, Departamento de Anestesiologia, Oncologia e Radiologia, Campinas, SP, Brasil.
[2]. Universidade Estadual de Campinas, Departamento de Neurologia, Campinas, SP, Brasil.
Corresponding author: Dr. Jean Levi Ribeiro de Paiva. e-mail: jeanlevirp@gmail.com
Authors’ contribution
JLRP: data acquisition and initial drafting of the manuscript.
TAMOC: critical revision of the manuscript for intellectual content.
FR: study conception, data acquisition, and critical revision of the manuscript for intellectual content.
Conflict of Interest
The authors declare that there is no conflict of interest.
Financial Support
There was no financial support for the preparation of this article.
Orcid
Jean Levi Ribeiro de Paiva: https://orcid.org/0000-0002-8109-9377
Tânia Aparecida Marchiori de Oliveira Cardoso: https://orcid.org/0000-0002-4565-3035
Fabiano Reis: https://orcid.org/0000-0003-2256-4379
A 15-year-old boy presented with a fever that lasted 50 days, with right eyelid edema and hyperemia, and a visual deficit diagnosed as chorioretinitis. One month later, the patient developed a brief episode of left hemiparesthesia and, subsequently, sudden paresis of the left upper and lower limbs without skin lesions. Cerebrospinal fluid (CSF) analysis revealed pleocytosis with a predominance of lymphocytes, restricting the differential diagnosis to viral infections, syphilis, inflammatory and autoimmune disease. The latter three were deemed unlikely after extensive laboratory analyses.
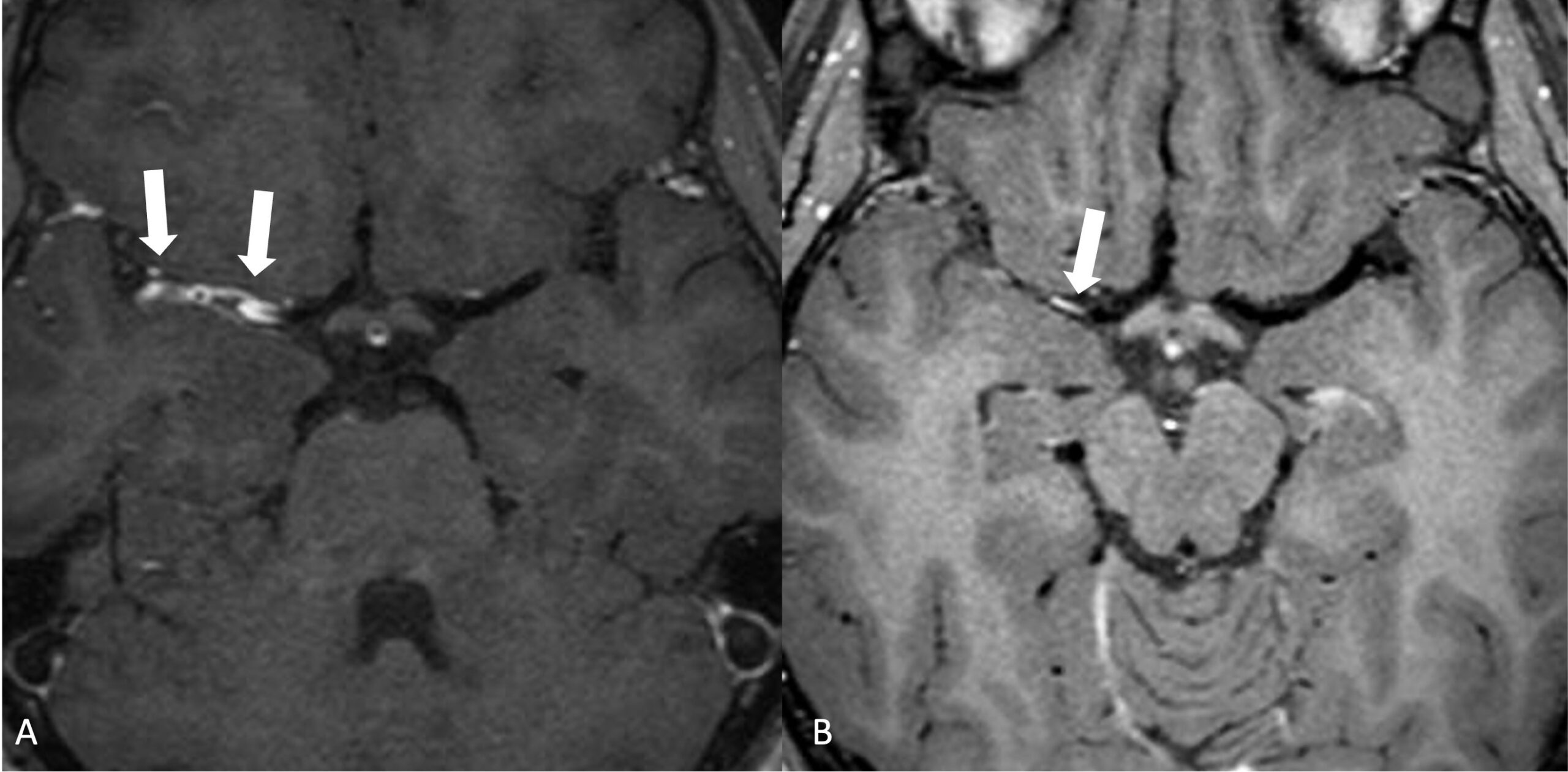
Magnetic resonance imaging (MRI) revealed lesions in the right basal ganglia, internal capsule, and deep white matter with restricted diffusion, consistent with acute ischemic stroke (Figure 1). Three-dimensional time-of-flight magnetic resonance angiography showed a lack of flow signal in the right middle cerebral artery (Figure 1), and high-resolution vessel wall imaging (HR-VWI) revealed concentric wall thickening with contrast enhancement in the right M1 and M2 segments, indicating vasculitis (Figure 2). Subsequent CSF analysis revealed elevated levels of IgG for the varicella zoster virus, and the patient was treated with acyclovir for 14 days. After treatment, HR-VWI showed a marked reduction in wall enhancement (Figure 2).
Herpes zoster ophthalmicus is associated with vasculopathy and cerebral infarction and has significant morbidity and mortality when untreated. Consequently, swift diagnosis is crucial but can be very challenging, especially in the absence of typical cutaneous lesions. In this context, MRI is a useful tool for diagnosing stroke and observing infectious vasculitis1,2,3.
Acknowledgments
We offer our deepest thanks to the institutions that provided technical support for the development and implementation of this study.
References
- Maher MD, Douglas VP, Douglas KAA, Collens SI, Gilbert AL, Torun N, et al. Clinical and neuroradiologic characteristics in varicella zoster virus reactivation with central nervous system involvement. J Neurol Sci. 2022;437:120262.
- Lau A, Essien EO, Tan IJ. Zoster sine herpete masquerading as central nervous system vasculitis. Cureus. 2020;12(3):e7231.
- Feitoza LM, Stucchi RSB, Reis F. Neurosyphilis vasculitis manifesting as ischemic stroke. Rev Soc Bras Med Trop. 2020;53:e20190546.
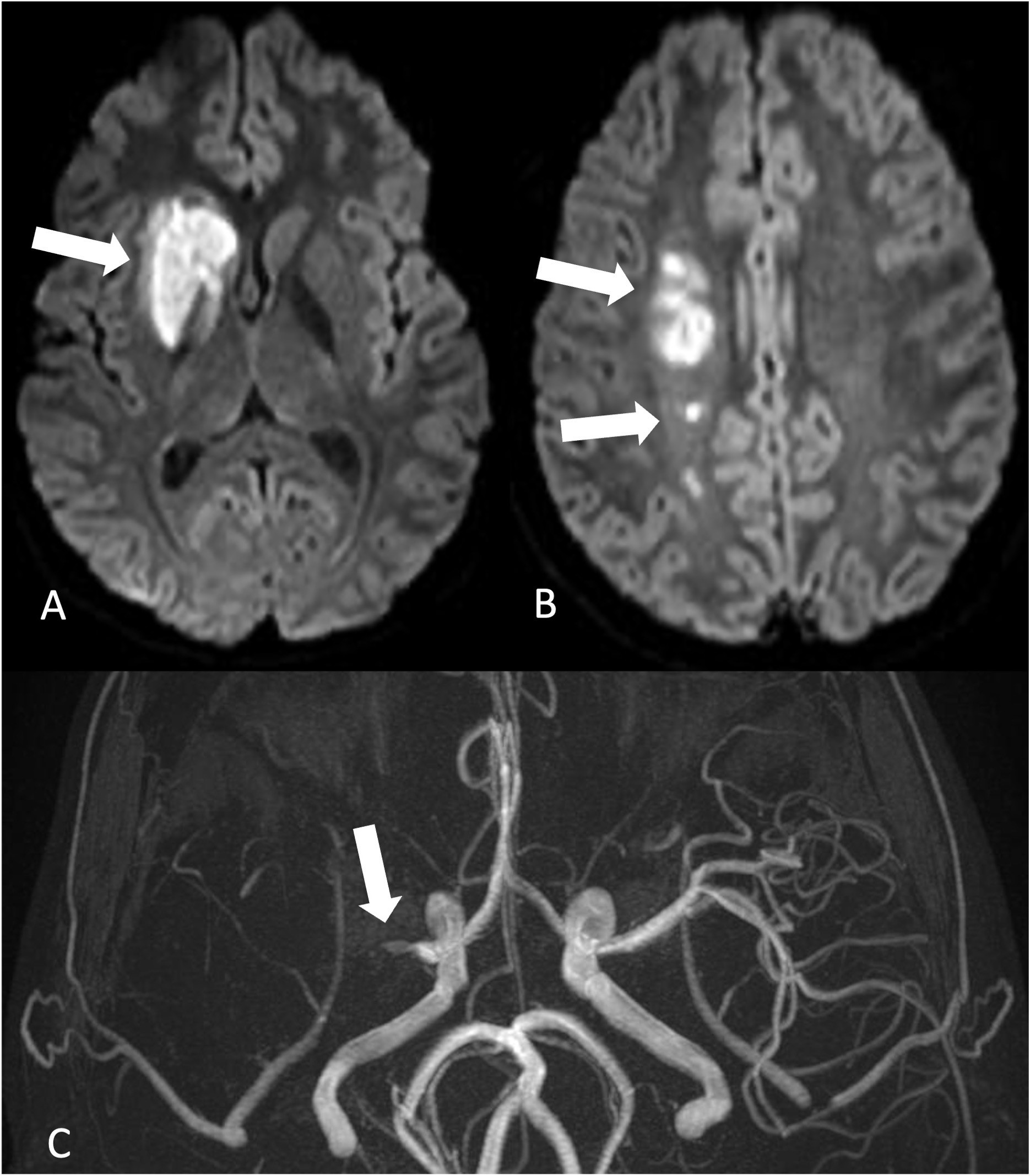
FIGURE 1: A and B. Axial diffusion-weighted images (DWI) showing right basal ganglia, internal capsule, and deep white matter hyperintensity (arrows), which had corresponding hypointensity on the apparent diffusion coefficient (ADC) map (not shown). This indicates restricted diffusion, consistent with acute ischemic stroke. C. Three-dimensional time-of-flight magnetic resonance angiography (3D-TOF) showing the absence of a flow signal in the right middle cerebral artery starting from its origin (arrow).
**Esta reportagem reflete exclusivamente a opinião do entrevistado.**