First report of an accident caused by Jaguajir agamemnon (C.L. Koch, 1839)
(Scorpiones, Buthidae) in Paraná state, Brazil
14/11/2023Kwasniewski FH et al. – Accident caused by Jaguajir agamemnon
Fábio Henrique Kwasniewski[1], Emanuel Marques da Silva[2], Edmarlon Girotto[3], Denise Maria Candido[4], Miriam de Cássia Tóffolo[5], Daniel Emilio Dalledone Siqueira[6], Luiz Roberto Costa Gomes[7] and Camilo Molino Guidoni[3]
[1]. Universidade Estadual de Londrina, Centro de Ciências Biológicas, Departamento de Ciências Patológicas, Londrina, PR, Brasil.
[2]. Secretaria de Estado da Saúde do Paraná, Laboratório de Taxonomia de Animais Peçonhentos, Curitiba, PR, Brasil.
[3]. Universidade Estadual de Londrina, Centro de Ciências da Saúde, Departamento de Ciências Farmacêuticas, Londrina, PR, Brasil.
[4]. Instituto Butantan, Biotério de Artrópodes, São Paulo, SP, Brasil.
[5]. Universidade Estadual de Londrina, Hospital Universitário, Centro de Informação e Assistência Toxicológica, Londrina, PR, Brasil.
[6] Secretaria de Estado da Saúde do Paraná, Centro de Informação e Assistência Toxicológica, Curitiba, PR, Brasil.
[7]. Prefeitura Municipal de Entre Rios do Oeste, Entre Rios do Oeste, PR, Brasil.
Corresponding authors: Fábio Henrique Kwasniewski. e-mail: fhkwas@uel.br; Camilo Molino Guidoni. e-mail: camiloguidoni@uel.br
Authors’ contribution
FHK: Conception and design of the study, analysis and interpretation of data, drafting the article, final approval of the version to be submitted.
EMS: Conception and design of the study, analysis and interpretation of data, drafting the article, final approval of the version to be submitted.
EG: Conception and design of the study, analysis and interpretation of data, drafting the article, final approval of the version to be submitted.
DMC: Conception and design of the study, analysis and interpretation of data, drafting the article, final approval of the version to be submitted.
MCT: Acquisition of data, conception and design of the study, final approval of the version to be submitted.
DEDS: Conception and design of the study, analysis and interpretation of data, drafting the article, final approval of the version to be submitted.
LRCG: Acquisition of data, final approval of the version to be submitted.
CGM: Conception and design of the study, analysis and interpretation of data, drafting the article, final approval of the version to be submitted.
Conflict of Interest
The authors declare that there is no conflict of interest.
Financial Support
The study lacked financial funding.
Orcid
Fábio Henrique Kwasniewski: https://orcid.org/0000-0002-0282-9096
Emanuel Marques da Silva: https://orcid.org/0009-0007-5677-4119
Edmarlon Girotto: https://orcid.org/0000-0001-9345-3348
Denise Maria Candido: https://orcid.org/0000-0001-6737-2106
Miriam de Cássia Tóffolo: https://orcid.org/0009-0004-6365-5191
Daniel Emilio Dalledone Siqueira: https://orcid.org/0000-0002-4421-3505
Luiz Roberto Costa Gomes: https://orcid.org/0009-0003-0038-2045
Camilo Molino Guidoni: https://orcid.org/0000-0001-5844-143X
Received 28 June 2023 – Accepted 29 September 2023
ABSTRACT
We report the first pediatric case of a Jaguajir agamemnon scorpion sting. This case occurred in the state of Paraná and is the first record of this species in southern Brazil. The patient was admitted within 15 min, with pain, local edema, erythema, whole-body pruritus, and tongue paresthesia within the first two hours, which disappeared thereafter. The patient’s condition was considered mild, with a positive outcome, and she recovered completely.
Keywords: Scorpion stings. Jaguajir agamemnon. Child.
INTRODUCTION
Scorpions are venomous animals that cause numerous human envenomations, especially in the poorest countries. Medically important stings are mainly caused by scorpions belonging to the Buthidae family, particularly those in the genus Tityus in South America1. In Brazil, mild accidents are typically characterized with local clinical manifestations, including pain, erythema, and edema, and sometimes with signs related to pain, such as mild tachycardia, nausea, and agitation. In moderate accidents, the systemic manifestations include sweating, nausea, vomiting, tachypnea, agitation, tachycardia, and hypertension. Severe envenomation is reported when such manifestations are intense, and others may be present, such as excessive salivation and sweetening, tachydyspnea, cardiac arrhythmias, hyper- or hypotension, agitation and prostration, convulsions, and muscle spasms, with progression to cardiogenic and respiratory shock causing death2.
Recently, scorpions have been involved in several accidents involving venomous animals in Brazil, posing an important public health issue. Most recorded accidents were caused by T. serrulatus, T. bahiensis, and T. stigmurus, which have similar clinical characteristics. When compared to the victims of any Tityus, who are generally implicated in mild accidents, people stung by T. serrulatus are at a higher risk of being included in moderate and severe accidents, particularly children aged 0–9 years, where lethality is also higher3.
Accidents involving different species of Tityus have been reported, especially in the northern area of the country, with symptoms distinct from those cited earlier4-6. However, stings have not been reported in other Buthidae scorpions. The new genus Jaguajir was created, and the species Rhopalurus agamemnon (C.L. Koch, 1839), Rhopalurus pintoi (Mello-Leitão, 1932), and Rhopalurus rochae (Borelli, 1910) were included as Jaguajir agamemnon (C.L. Koch, 1839), Jaguajir pintoi (Mello-Leitão, 1932), and Jaguajir rochae (Borelli, 1910), respectively7. They are commonly found in the north-eastern, mid-western, and northern regions of the Brazilian Cerrado.
Case descriptions of envenomation caused by Jaguajir agamemnon are extremely rare, and searches in the most used databases (Cochrane Library, LILACS, SciELO, Scopus, Redalyc, MedLine, and PubMed Central) showed no more than two articles describing accidents in adults living in the natural habitat of this scorpion. However, in only one case, the animal was properly identified8,9. Here, we report a pediatric case of J. agamemnon-induced envenomation in a small city in Paraná, southern Brazil.
CASE REPORT
The accident occurred in February 2023 during the summer, involving a 6-year-old female child who was stung on the dorsum of the right foot while playing in her home in the urban area of the small city of Entre Rios do Oeste (24º42’14’’S, 54º14’32’’O), state of Paraná, in the South region of Brazil. The case was monitored via teleservice by the Center for Information and Toxicological Assistance of Londrina at the University Hospital of the State University of Londrina (CIATox-Londrina), a regional reference health service that provides 24-hour phone support or bedside consultations for toxicology and accidents, along with venomous animal clinical case management.
The patient received the first medical care within 15 minutes in a Basic Health Unit (BHU) with intense pain and local signs of a sting surrounded by edema and erythema (Figure 1A). A local anesthetic blockade was performed, and the patient was referred to a medical clinic when contact with CIATox-Londrina was established. At this point, 30 min had elapsed since the sting. Analgesics were not administered, as the patient did not complain of any pain. Cleaning the injured site and verifying the vaccination card for tetanus is advised. In addition, the patient should be observed for at least 6 h with special attention to clinical manifestations such as sweating, agitation, tachycardia, hypertension, nausea, vomiting, and salivation. Approximately one hour after the sting, a small hematoma was observed at the sting site (Figure 1B).
Whole-body pruritus and tongue paresthesia resolved spontaneously two hours after the incident report, after which no further symptoms were observed. Between 2 and 4 h after the sting, the patient presented with stable health, with a mean arterial pressure of 90/60 mmHg, heart rate of 112–120 beats per minute, and oxygen saturation of 99%. The patient was continuously observed every 30 min before being discharged seven hours after she was admitted to the clinic. The patient’s condition was classified as mild and recovered fully. One day after the accident, the foot was swollen and erythematous (Figure 1C), and cold water compression was applied to relieve the edema. On the third day, erythema (Figure 1D) remained, and persistent tingling was observed in the toes.
The scorpion was captured by the family and sent to a municipal environmental health surveillance facility, which then forwarded its image for identification to the Venomous Animals Taxonomy Laboratory of the Center of Information and Toxicological Assistance of Paraná. It was identified as Jaguajir agamemnon (Figure 2).
DISCUSSION
We are not aware of any pediatric case reports caused by J. agamemnon, making this the first report. In the State of Paraná, T. bahiensis, T. serrulatus, T. costatus, Bothriurus, and Ananteris spp. are frequently found. The State Program for the Surveillance of Accidents by Venomous and Poisonous Animals recorded two specimens of J. agamemnon in the 1990s from municipalities in the West that were never found again apart from sporadic cases of passive transport. Interestingly, the patient’s father was a truck driver who had recently traveled to the northeastern region of the country. One study reported the occurrence of J. rochae, an animal adapted to the same biome as J. agamemnon, in the city of São Paulo (state of São Paulo, Southeastern Brazil), possibly arriving in boxes of melon10.
Although this case occurred in a child, it has some similarities with a previously published case regarding an adult who was stung by J. agamemnon in the state of Bahia, in the northeastern region of Brazil. Mild pain with intense local pruritus was reported, and after one hour, whole-body paresthesia with greater intensity was observed in the tongue and extremities9. Pruritus was present in our case but in the whole body, as well as paresthesia on the tongue. In our case, pain, local edema, and erythema were present soon after the sting; however, the edema and erythema persisted for up to three days. Although CIATox-Londrina pain was not reported at the time of follow-up, local anesthetic blockade was initially administered during the first visit to the BHU. One of the reasons why this type of approach to relieving local pain is no longer indicated is that it has a short-lived effect, and because the use of analgesics is no longer necessary, the pain is probably less intense.
This case and the one reported in Bahia9 were considered mild, while accidents involving an 18-year-old man and an adult woman caused by J. agamemnon in Piauí, northeast region, were considered moderate. In both cases, the local pain was intense, spreading to the shoulder in the young man; signs of systemic effects such as agitation, salivation, lacrimation, blurred vision, muscle spasms, tachycardia, and hypotension in the woman; and somnolence and salivation in the young man. Anti-scorpionic serum was prescribed in both cases. The scorpion was not captured at the time of these accidents; however, in the case of the female, it was captured afterward during a search of the surroundings of her property. In a case involving a young man, the animal was only described by the victim8.
Two more cases are documented in specialized literature with Rhopalurus, both in male adults living in the state and in the northeastern region of Brazil. In cases where the victim was stung by R. amazonicus (currently R. laticauda7), local pain spread to the arm and paresthesia was felt11. In the case involving J. rochae, after starting with mild pain, the patient developed fatal anaphylaxis, as evidenced by autopsy findings of the glottis and pulmonary edema, and based on his history of allergy triggered by a bee sting and contact with beetles and crabs12.
In conclusion, cases involving J. agamemnon have rarely been reported. In addition to being described as the only pediatric case caused by this scorpion, this is the first reported case outside the northeast region. Although the outcome in our case was positive, more attention should be paid when the victim is a child, as moderate envenomation in adults has been previously reported.
Acknowledgments
The authors would like to express their sincere gratitude to the patient’s parents for sharing accident data and providing the essential photographs for our study.
References
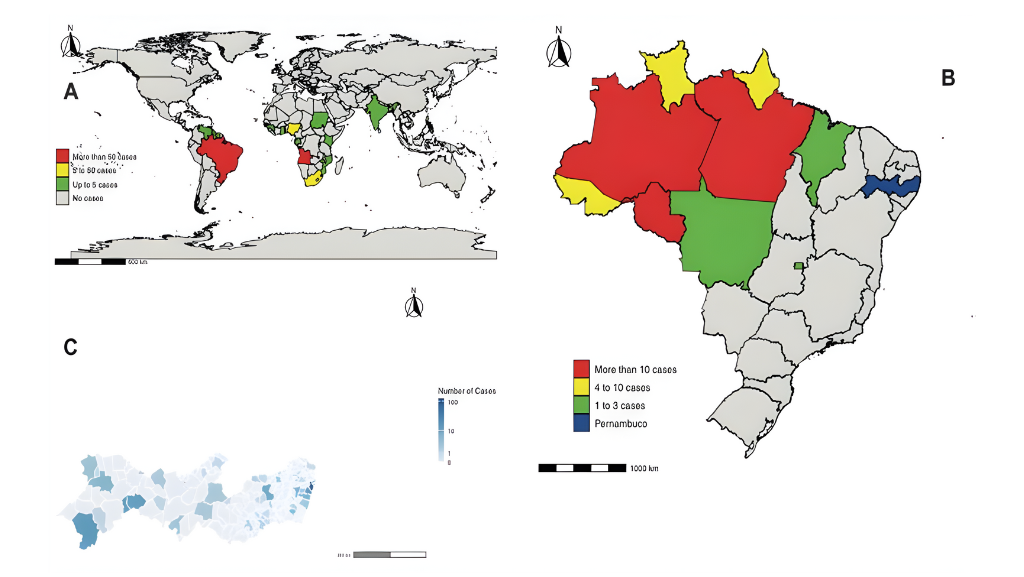
- Chippaux J-P, Goyffon M. Epidemiology of scorpionism: A global appraisal. Acta Trop. 2008;107(2):71-9.
- Cupo P. Clinical update on scorpion envenoming. Rev Soc Bras Med Trop. 2015;48(6):642-9.
- Guerra-Duarte C, Saavedra-Langer R, Matavel A, Oliveira-Mendes BBR, Chavez-Olortegui C, Paiva ALB. Scorpion envenomation in Brazil: Current scenario and perspectives for containing an increasing health problem. PLoS Negl Trop Dis. 2023;17(2):e0011069.
- Pardal PPO, Ishikawa EAY, Vieira JLF, Coelho JS, Dórea RCC, Abati PAM, et al. Clinical aspects of envenomation caused by Tityus obscurus (Gervais, 1843) in two distinct regions of Pará state, Brazilian Amazon basin: a prospective case series. J Venom Anim Toxins Incl Trop Dis. 2014;20:52-9.
- Coelho JS, Ishikawa EAY, Santos PRSG, Pardal PPO. Scorpionism by Tityus silvestris in Eastern Brazilian Amazon. J Venom Anim Toxins Incl Trop Dis. 2016;22:24-8.
- Silva BAJ, Fé NF, Gomes AAS, Souza AS, Sachett JAG, Fan HW, et al. Implication of Tityus apiacas (Lourenco, 2002) in Scorpion envenomations in the Southern Amazon border, Brazil. Rev Soc Bras Med Trop. 2017;50(3):427-30.
- Esposito LA, Yamaguti HY, Souza CA, Pinto-da-Rocha R, Prendini L. Systematic revision of the neotropical club-tailed scorpions, Physoctonus, Rhopalurus, and Troglorhopalurus, revalidation of Heteroctenus, and descriptions of two new genera and three new species (Buthidae: Rhopalurusinae). Bull Am Mus Nat Hist. 2017;415:1-136.
- Carvalho LS, Santos MPD, Dias SC. Scorpionism in the rural zone of Teresina, State of Piauí: relate of envenomation cases. Rev Soc Bras Med Trop. 2007;40(4):491.
- Brandão RA, Françoso RD. Accident caused by Rhopalurus agamemnon (Koch, 1839) (Scorpiones, Buthidae). Rev Soc Bras Med Trop. 2010;43(3):342-4.
- Bertani R, Bonini RK, Toda MM, Isa LS, Figueiredo JVA, Santos MR, et al. Alien scorpions in the Municipality of São Paulo, Brazil – evidence of successful establishment of Tityus stigmurus (Thorell, 1876) and first records of Broteochactas parvulus Pocock, 1897, and Jaguajir rochae (Borelli, 1910). Bioinvasions Rec. 2018;7(1):89-94.
- Fuentes-Silva D, Santos-Jr AP, Oliveira JS. Envenomation caused by Rhopalurus amazonicus Lourenco, 1986 (Scorpiones, Buthidae) in Para State, Brazil. J Venom Anim Toxins Incl Trop Dis. 2014;20:52-61.
- Melo IMLA, Ramalho RD, Bezerra MMV, Filho IEO, Medeiros CR, Gadelha MAC, et al. Fatal anaphylaxis to Jaguajir rochae (Borelli, 1910) (Scorpiones, Buthidae) in Brazil: a case report. Rev Patol Trop. 2019;48(3):187-94.

FIGURE 1: Images of the sting showing local edema and erythema (A), a small area of hematoma in the local area of the sting and large erythema on the dorsum (B), a swollen foot 24 h after the accident (C), and persistent erythema on the dorsum of the foot 3 days later (D).

FIGURE 2: Images of the scorpion involved in the accident, identified as Jaguajir agamemnon.