Paediatric Splenic Abscess Due to Salmonella
Memis KB et al. - Paediatric Salmonella-Induced Splenic Abscess
12/08/2024Kemal Buğra Memiş[1], Zeynep Betul Deve[1] and Sonay Aydın[1]
[1]. Erzincan University, School of Medicine, Department of Radiology ,Erzincan, Turkey.
Corresponding author: Kemal Bugra Memis, MD. e-mail: kemalbugramemis@gmail.com
Authors’ contribution
KBM: Conceptualization, Formal analysis, Investigation, Methodology ,Supervision, Writing review and editing, Writing original draft; ZBD: Methodology Software, Visualization, Writing original draft; SA:Methodology,Conceptualization,Formalanalysis,Investigation, Supervision, Validation, Writing review and editing;
Conflict of Interest
The authors declare no conflict of interest.
Financial Support
This research received no external funding.
Orcid
Kemal Bugra Memis: https://orcid.org/0009-0007-6746-3906
Zeynep Betul Deve: https://orcid.org/0009-0003-9159-0981
Sonay Aydın: https://orcid.org/0000-0002-3812-6333
Received 15 March 2024 – Accepted 23 May 2024
A 12-year-old boy presented to the emergency department with upper left quadrant abdominal pain, fever, and vomiting for three days. He had a fever of 38.5 °C. Test results revealed an elevated white blood cell count and C-reactive protein level.
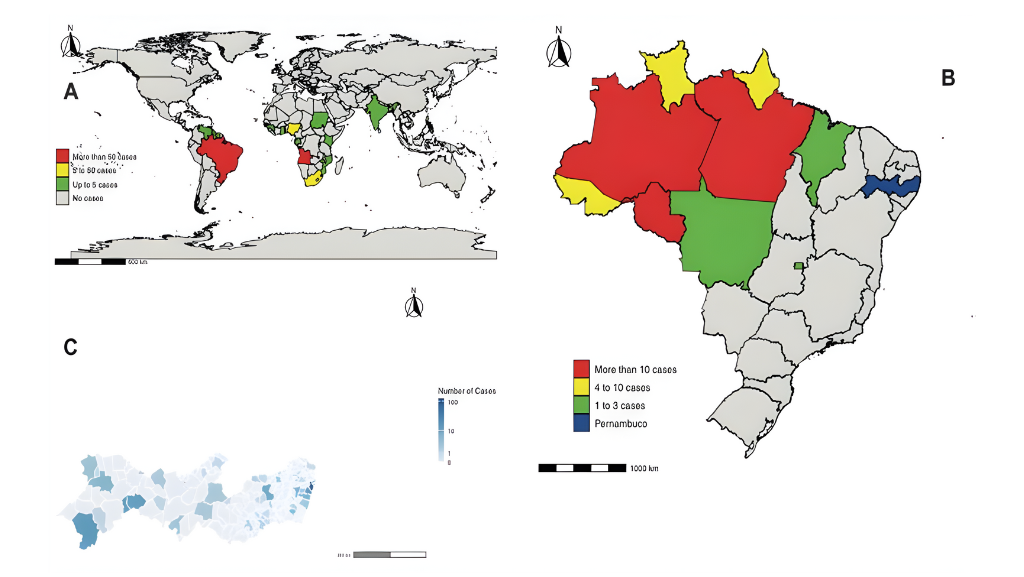
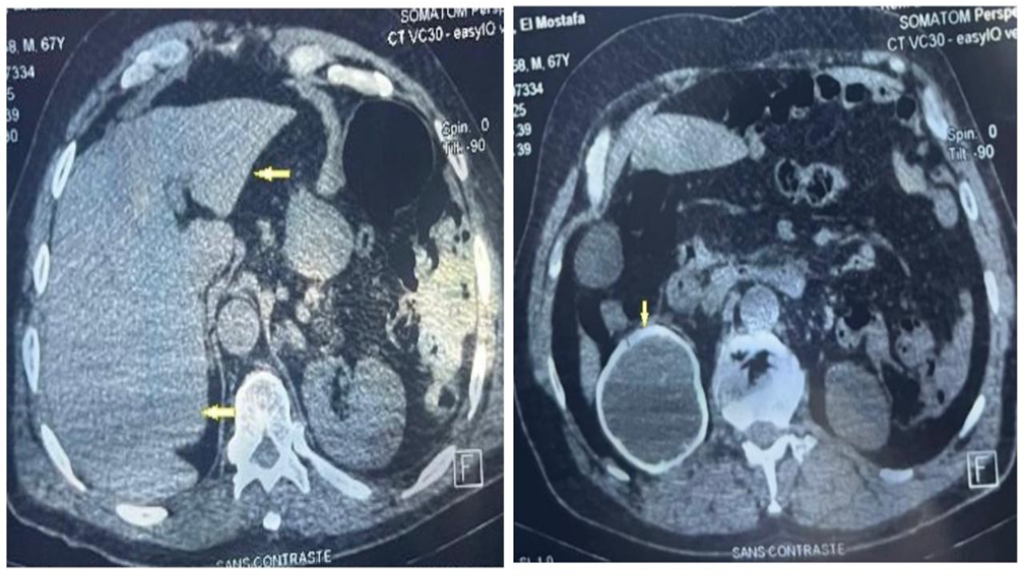
Computed tomography (CT) revealed a thick-walled cystic lesion measuring approximately 11 cm across the spleen. The patient experienced septation and wall calcification on the upper side. A 2-cm depth of pelvic free fluid was also found (Figure 1). Percutaneous drainage and an 8-day antibiotic regimen were administered, and Salmonella type B was cultured from the abscess. The symptoms improved, leading to discharge. Follow-up CT revealed a 7 × 5-cm septate collection area extending into the splenogastric recess, compressing the stomach’s greater curvature and causing inflammatory wall thickening with perisplenic free fluid, suggestive of a hematoma (Figure 2). Following discharge, the hematoma, which was monitored using ultrasonography in our radiology department, was completely absorbed.
Splenic abscesses are rare in children and are associated with high mortality rates. The reported incidence in autopsy series ranges from 0.14%–0.7%1. Symptoms such as fever and abdominal pain are nonspecific. Increased imaging allows for early diagnosis, which is crucial. Aerobic microorganisms, including staphylococci, streptococci, salmonella, and Escherichia coli, are common2. Percutaneous drainage, preferred over surgery, yields 51–72% success rates under specific conditions, replacing traditional antibiotic therapy and splenectomy3,4. This case highlights the importance of considering splenic abscesses in the differential diagnosis of children presenting with nonspecific symptoms such as fever and abdominal pain.
Acknowledgements
The authors thank the research staff at the Radiology Department of Erzincan University for their valuable assistance.
References
- Faruque AV, Qazi SH, Arshad M, Anwar N. Isolated splenic abscess in children, role of splenic preservation. Pediatr Surg Int. 2013;29(8):787–90.
- Liu YH, Liu CP, Lee CM. Splenic abscesses at a tertiary medical center in Northern Taiwan. J Microbiol Immunol Infect. 2014;47(2):104–8.
- Qu J, Zong Z. Giant splenic cyst complicated by infection due to Salmonella enterica serovar Livingstone in a previously healthy adolescent male: a case report. BMC Infect Dis. 2022;22(1):557.
- Thanos L, Dailiana T, Papaioannou G, Nikita A, Koutrouvelis H, Kelekis DA. Percutaneous CT-guided drainage of splenic abscess. AJR Am J Roentgenol. 2002;179(3):629–32.

FIGURE 1: Axial- (A), coronal- (B) and sagittal–plane (C) abdominal CT showing a thick-walled hypodense cystic lesion approximately 11 cm in diameter in the spleen, with septations and wall calcification in the superior aspect (white arrows); axial- (D) and coronal-plane (B) abdominal CT showing free fluid of approximately 2 cm depth in the pelvic area (blue arrow).
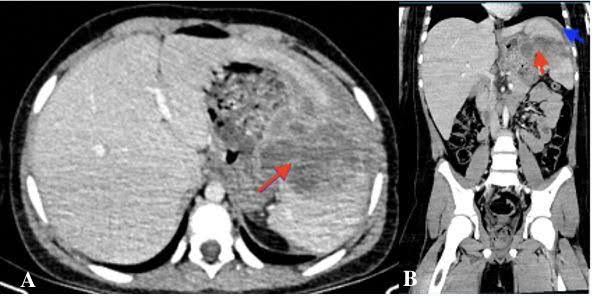
FIGURE 2: Axial- (A) and coronal-plane (B) CT images of a hematoma occurring in the perisplenic region one month after the drainage. 7×5-cm septated and wall-enhancing collection area, extending into the splenogastric recess (red arrows); free fluid measuring 15 mm in depth in the perisplenic space (blue arrow).