Persistent cervical infection with the Chikungunya virus
Chikungunya virus was detected in the cervix of two women up to six months post-infection. Findings highlight viral persistence and the need to investigate other tissue reservoirs
05/05/2025
Chikungunya virus E2 protein (green) detected in cervical cells. Nuclei stained red or blue. Case A: asymptomatic; Case B: symptomatic. Magnification: 100X
Pérez-Pérez JE et al. – Chikungunya virus and cervix
José Eduardo Pérez-Pérez[1],[2], Oscar Guzmán-Martínez[1],[3], Jesús Miguel Torres-Flores[4], Clara Luz Sampieri[1], Julio Isael Pérez-Carreón[5], Nayali López-Balderas[6], Miguel Ángel Barragán[7], José Guillermo Mendoza-Cervantes[8], Fabio García-García[2], Alma Campos[1], David Sánchez-Marí[9] and Hilda Montero[1]
[1]. Instituto de Salud Pública, Universidad Veracruzana, Xalapa, Veracruz, México.
[2]. Instituto de Ciencias de la Salud, Universidad Veracruzana, Xalapa, Veracruz, México.
[3]. Centro de Investigaciones Biomédicas, Universidad Veracruzana, Xalapa, Veracruz, México.
[4]. Instituto Politécnico Nacional, Cuidad de México, México.
[5]. Instituto Nacional de Medicina Genómica, Cuidad de México, México.
[6]. Instituto de Medicina Forense, Universidad Veracruzana, Boca del Río, Veracruz, México.
[7]. Hospital de Alta Especialidad de Veracruz, Veracruz, Veracruz, México.
[8]. Centro de Investigación en Micología Aplicada, Universidad Veracruzana, Xalapa, Veracruz, México.
[9]. Facultad de Medicina, Universidad Nacional Autónoma de México (UNAM), Ciudad de México, México.
Corresponding author: Dr. Hilda Montero. e-mail: hmontero@uv.mx
Authors’ contribution
JEPP: Formal analysis, Methodology, Writing – original draft. OGM: Formal analysis, Methodology, Writing – original draft. JMTF: Formal analysis, Resources, Writing – review & editing. CLS: Formal analysis, Methodology, Validation, Writing – review & editing. JIPC: Formal analysis, Writing – original draft, Writing – review & editing. NLB: Investigation, Methodology, Writing – review & editing. MAB: Investigation, Methodology, Resources. GMC: Formal analysis, Resources, Writing – review & editing. FGG: Formal analysis, Supervision, Writing – review & editing. AC: Data curation, Investigation, Writing – review & editing. DSM: Data curation, Investigation, Writing – review & editing. HM: Conceptualization, Formal analysis, Funding acquisition, Investigation, Resources, Supervision, Writing – original draft.
Conflict of Interest
The authors declare no conflict of interest.
Financial Support
This research was partially funded by Instituto de Salud Pública, Universidad Veracruzana.
Orcid
José Eduardo Pérez-Pérez: https://orcid.org/0000-0003-1221-4498
Oscar Guzmán-Martínez: https://orcid.org/0000-0003-4150-0696
Jesús Miguel Torres-Flores: https://orcid.org/0000-0002-2194-521X
Clara Luz Sampieri: https://orcid.org/0000-0001-7495-426X
Julio I. Pérez-Carreón: https://orcid.org/0000-0001-9284-7775
Nayali López-Balderas: https://orcid.org/0000-0002-0996-6966
Miguel Ángel Barragán: https://orcid.org/0009-0004-1288-2634
Guillermo Mendoza-Cervantes: https://orcid.org/0000-0002-4828-225X
Fabio García-García: https://orcid.org/0000-0002-3756-9845
Alma Campos: https://orcid.org/0000-0003-1750-5171
David Sánchez-Marín: https://orcid.org/0000-0002-8525-3810
Hilda Montero: https://orcid.org/0000-0001-8090-4103
Abstract
Chikungunya virus (CHIKV) induces an acute infection known as chikungunya fever; however, the persistence of CHIKV infections has been reported. This report investigated the persistence of CHIKV over six months in the cervix of two infected women. The infectious CHIKV was isolated from three samples. Our findings demonstrated the persistence of CHIKV in the cervix, highlighting the importance of evaluating other tissue types.
Keywords: Chikungunya virus. viral persistence. cervix.
Introduction
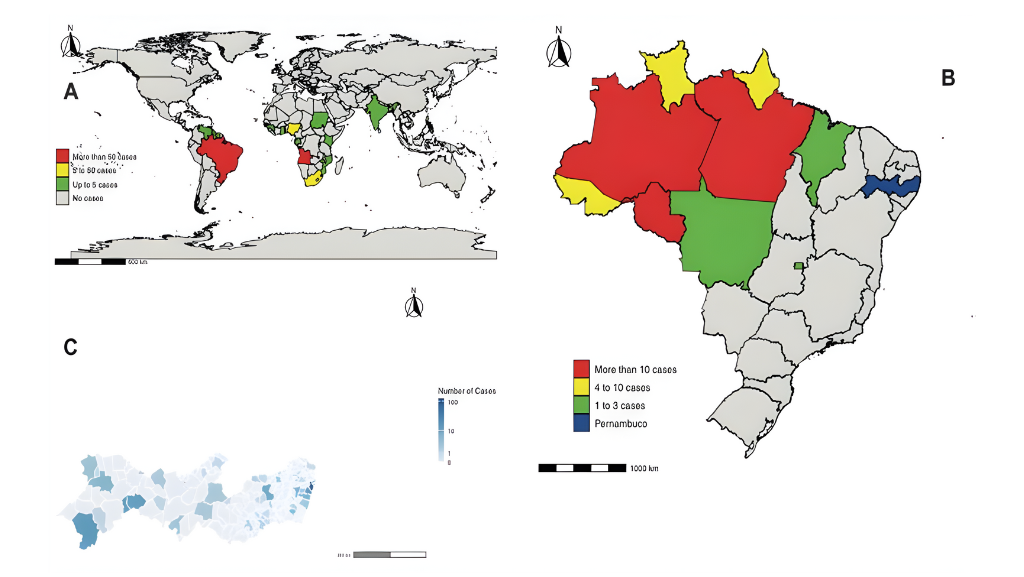
First described in 1952 during an outbreak of febrile illness in Tanzania1, Chikungunya virus (CHIKV) is an arthropod-borne virus (arbovirus) belonging to the Alphavirus genus of the Togaviridae family2. Mature CHIKV particles are enveloped, containing a single-stranded RNA genome of approximately 12 kb in length1,2.
The CHIKV is mainly transmitted through the bite of infected female Aedes mosquitoes. This vector, as well as Aedes aegypti and Aedes albopictus3, has been implicated in the transmission cycle of this virus in urban and peri-urban areas. Viral replication commences in the dermal fibroblasts once an infected mosquito bites a vertebrate host; the virus proliferates before entering the bloodstream. The target cells of CHIKV include monocytes, hepatocytes, chondrocytes, endothelial cells, fibroblasts, and myocytes2,3,4.
CHIKV infection leads to chikungunya fever, which is symptomatic in 85% of cases. The acute phase of the disease is characterized by the presence of fever, arthralgia/arthritis, fatigue, myalgia, nausea, and vomiting. The development of a generalized maculopapular rash has been reported in some cases2. Persistence of CHIKV infections has not been thoroughly characterized. However, several reports have indicated the presence of CHIKV-like symptoms in 30–40% of patients2,4, highlighting its prevalence in public health systems. The persistence of CHIKV infections years after the first infection has also been reported, with persistence in the bone and joint tissues, the common sites of CHIKV persistence, triggering rheumatoid arthritis and ankylosing spondylitis3,4.
Although CHIKV is commonly transmitted through the bites of infected mosquitoes, vertical transmission has also been reported5. Notably, CHIKV RNA has been detected in the semen and vaginal fluid of infected patients during the acute phase of the disease4; however, CHIKV has been persistently detected in semen6,7,8.
The persistence of CHIKV RNA and E2 protein was analyzed in the cervical samples acquired from one asymptomatic woman and one woman with symptoms consistent with chikungunya fever in the present study. The databases of Cochrane Library, LILACS, SciELO, MEDLINE, PubMed, and PubMed Central (PMC) were searched to retrieve publications addressing the persistence of CHIKV in the cervix. However, no such publications could be retrieved, indicating that this is the first study on this subject.
Case Report
Case 1 was an asymptomatic 60-year-old woman who was the sexual partner of a male patient diagnosed with ZIKV infection through RT-PCR. The patient had no comorbidities or a history of symptoms compatible with arboviruses. The patient was not receiving any medications at the time of the study. Serological analysis revealed negative anti-CHIKV IgM antibodies, but positive anti-CHIKV IgG antibodies. The patient also tested positive for anti-ZIKV IgG antibodies and negative for anti-ZIKV IgM, anti-DENV IgM, and anti-DENV IgG antibodies.
Case 2 was a symptomatic 26-year-old woman with acute CHIKV infection at the time of enrollment in the study. The patient presented with arthralgia, fever of 39.5 ºC persisting for 2–3 days, loss of appetite, dizziness, and exanthema. CHIKV was detected in the serum and urine samples of this patient through endpoint RT-PCR. The patient had no comorbidities and was not receiving any medication at the time.
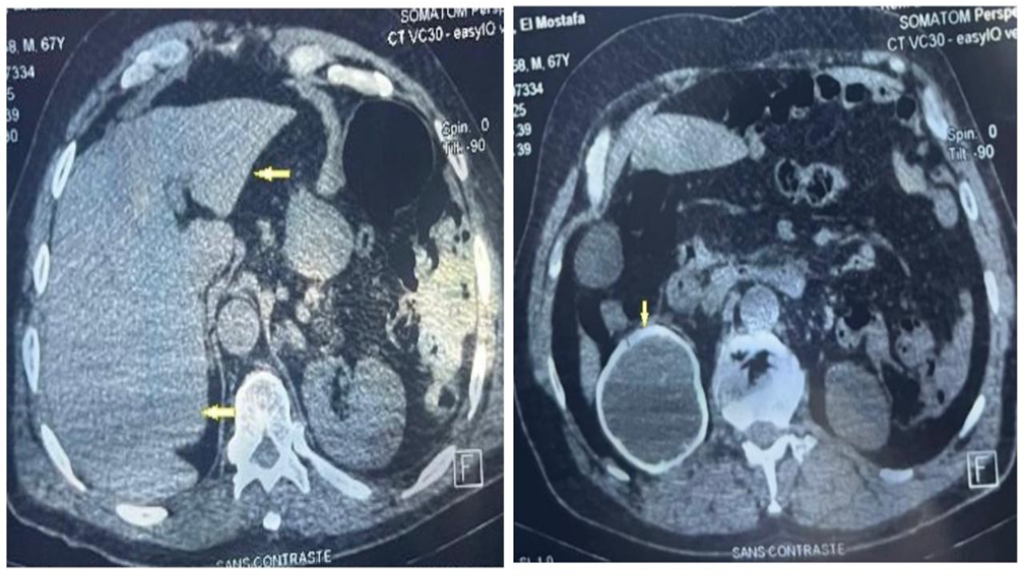
Cervical scrapings were obtained longitudinally from both patients at 0, 4, 6, and 10 months. For Case 1, time 0 corresponds to the time-point the patient was enrolled in the study. For case 2, time 0 corresponded to the sample acquired 21 days after the onset of the symptoms of chikungunya fever. No macroscopic lesions were observed during sample collection; only data associated with inflammation were obtained. The patients did not report any gynecological symptoms.
A smear from the cervical scrapings was used to detect CHIKV E2 protein using immunofluorescence assays. The cervical cytobrush was placed in Leibovitz viral transport media (11415056, Gibco, UK) containing antibiotics and an antimycotic after obtaining the smear and kept frozen at -80 ºC for further use in RNA viral detection and viral isolation.
Detection of E2 protein of CHIKV in cervix
The E2 protein of CHIKV in all cervical samples (up to the 6-month sample) acquired from the two patients was detected through immunofluorescence assays conducted using an anti-E2 antibody (MAB12130-200; Native Antigen Company, UK). Figure 1 presents a representative image. The 10-month sample could not be analyzed in either case.
RNA viral detection
CHIKV RNA was obtained from the total RNA extracted from cervical scraping samples using the QIAamp Viral RNA Mini Kit (52906, QIAGEN, USA) in accordance with the manufacturer’s instructions. Endpoint RT-PCR assays were performed using a One-Step RT-PCR kit (210212; QIAGEN, USA). Real-time RT-PCR was performed using a ZDC Multiplex RT-PCR Assay (12003818, Bio-Rad, USA).
CHIKV RNA was detected through endpoint RT-PCR in all samples acquired up to the 4-month time-point in case 1. At the same time, viral RNA was detected through real-time RT-PCR in case 2. The time of infection was unknown as Case 1 did not exhibit any signs or symptoms; therefore, the maximum duration of persistence could have been longer. Sanger sequencing of the RT-PCR products was performed using the following CHIKV genome-specific oligonucleotides: forward primer sequence, TAGAGCAGGAAATTGATCCC; and reverse primer sequence, CTTTAATCGCCTGGTGGTGGTAT. Only one sample was sequenced and registered in the NCBI for Biotechnology Information database. Alignment was performed, and a 92% consistency with the CHIKV sequence was identified (Table 1).
Viral isolation
To assess the presence of the infectious virus in the samples, viral isolation procedures were carried out in Vero cells cultured in DMEM supplemented with antibiotics and antimycotics. The samples were lysed through cryofracture after 10 days, and viral RNA was extracted and detected using endpoint RT-PCR. Three samples, two from case 1 (4 and 6 months) and one from case 2 (6 months), were positive for CHIKV RNA after viral isolation, indicating the presence of infectious viral particles in the samples (Table 1).
Discussion
No previous study has reported the persistence of CHIKV in the cervix. Thus, the present study is the first study to report that cervical cells represent another location for the persistence of CHIKV. This aspect has remains to be explored and requires attention owing to the possible long-term effects of continuous viral replication, which could be similar to the complications observed in infected bone and joint tissues4. Consistent with the findings of the present study, CHIKV possesses ample tropism and that epithelial cells in the cervix express Matrix Remodeling-Associated 8 protein (MXRA8), a known receptor for CHIKV9,10.
The CHIKV E2 protein and RNA detected in the present study exhibited variability among the samples. This may be attributed to three different phenomena: 1) the differential distribution of sites of persistent CHIKV replication in the cervix, 2) the loss of viral and cellular material owing to the application of the smear technique, which resulted in the loss of viral RNA in the sample used for RT-PCR detection, and 3) low viral replication. The latter has been observed in other viruses, such as Zika, wherein the viral titer in the cervix was lower than that in the serum and urine samples11,12.
The detection of infectious viral particles in cervical samples highlights the risk of sexual transmission of CHIKV, as reported for other arboviruses such as the Zika virus or dengue11,13. This emphasizes the relevance of the findings of the present study and provides a basis for further research using larger samples and longer follow-up periods. Furthermore, the persistence of CHIKV in the cervix could be the cause of vertical transmission5 or abortion14, as recently reported, requires further investigation.
Ethical statement
This study was approved by the research and ethics committees of the corresponding institutions. The study began in July 2018, and both patients signed informed consent forms indicating their agreement to participate.
Acknowledgments
JEPP (#850483), and OGM (#718013) are recipients of a scholarship from the Consejo Nacional de Ciencia y Tecnología. We thank Elizabeth Martínez Castillo, Cirenia Hernández Trejo, Sobeida Blázquez and Gandhi Landa for their valuable technical assistance in this study; Susana López for providing the oligonucleotide sequences for CHIKV identification and CHIKV plasmids to be used as positive controls. We thank all participants for allowing us to take serial samples.
References
- de Lima Cavalcanti TYV, Pereira MR, de Paula SO, Franca RFO. A Review on Chikungunya Virus Epidemiology, Pathogenesis and Current Vaccine Development. Viruses. 2022;5;14(5):969.
- Schwartz O, Albert ML. Biology and pathogenesis of chikungunya virus. Nat Rev Microbiol. 2010;8(7):491-500.
- Silva LA, Dermody TS. Chikungunya virus: epidemiology, replication, disease mechanisms, and prospective intervention strategies. J Clin Invest. 2017;127(3):737-749.
- Matusali G, Colavita F, Bordi L, Lalle E, Ippolito G, Capobianchi MR, et al. Tropism of the Chikungunya Virus. Viruses. 2019;11(2).
- Villamil-Gomez W, Alba-Silvera L, Menco-Ramos A, Gonzalez-Vergara A, Molinares-Palacios T, Barrios-Corrales M, et al. Congenital Chikungunya Virus Infection in Sincelejo, Colombia: A Case Series. J Trop Pediatr. 2015;61(5):386-92.
- Bandeira AC, Campos GS, Rocha VF, Souza BS, Soares MB, Oliveira AA, Abreu YC, Menezes GS, Sardi SI. Prolonged shedding of Chikungunya virus in semen and urine: A new perspective for diagnosis and implications for transmission. IDCases. 2016 Nov 4;6:100-103.
- Feldmann H. Virus in semen and the risk of sexual transmission. N. Engl. J. Med. 2018;378:1440–1441. doi: 10.1056/NEJMe1803212.
- Martins EB, de Bruycker-Nogueira F, Rodrigues CDS, Santos CC, Sampaio SA, Fabri AA, Guerra-Campos V, Mares-Guia MAM, Faria NRC, Santos AS, Pinto MAS, Silva MFB, Moraes ICV, Pina-Costa A, Filippis AMB, Brasil P, Calvet GA. Chikungunya Virus Shedding in Semen: A Case Series. Viruses. 2022 Aug 26;14(9):1879.
- Song H, Zhao Z, Chai Y, Jin X, Li C, Yuan F, et al. Molecular Basis of Arthritogenic Alphavirus Receptor MXRA8 Binding to Chikungunya Virus Envelope Protein. Cell. 2019;177(7):1714-24 e12.
- Gene Bank, National Center for Biotechnology Information. MXRA8 matrix remodeling associated 8 [Homo sapiens (human). [Accessed 6 May 2020]. Available from: https://www.ncbi.nlm.nih.gov/gene?term=(mxra8[gene])%20AND%20(Homo%20sapiens[orgn])%20AND%20alive[prop]%20NOT%20newentry[gene]&sort=weight.
- da Cruz TE, Souza RP, Pelloso SM, Morelli F, Suehiro TT, Damke E, et al. Case Reports: Prolonged Detection of Zika Virus RNA in Vaginal and Endocervical Samples from a Brazilian Woman, 2018. Am J Trop Med Hyg. 2019;100(1):183-6.
- Read JS, Torres-Velasquez B, Lorenzi O, Rivera Sanchez A, Torres-Torres S, Rivera LV, et al. Symptomatic Zika Virus Infection in Infants, Children, and Adolescents Living in Puerto Rico. JAMA Pediatr. 2018;172(7):686-93.
- Lee C, Lee H. Probable female to male sexual transmission of dengue virus infection. Infect Dis. 2019;51(2):150-2.
- Salomão N, Brendolin M, Rabelo K, Wakimoto M, de Filippis AM, Dos Santos F, Moreira ME, Basílio-de-Oliveira CA, Avvad-Portari E, Paes M, Brasil P. Spontaneous Abortion and Chikungunya Infection: Pathological Findings. Viruses. 2021;13(4):554.

FIGURE 1: The E2 viral protein of chikungunya virus (CHIKV) detected in the cervical cells. The cells were fixed with reactive-grade acetone at 4°C for 1 minute and stained with an antibody targeting the E2 protein (green). The cellular nuclei were stained with propidium iodide (red) or DAPI (blue). Case 1: asymptomatic patient (A), case 2: symptomatic patient (B). A representative image of a field with cells positive to the detection of E2 is shown (100X magnification).
TABLE 1: Chikungunya virus detected in the cervical tissue.
| Sample number | Time
(months) |
Endpoint RT-PCR | Smear/
Immunoreactivity |
Viral culture
RT-PCR |
Real-time RT-PCR | Sequency | ||
| Case 1
Asymptomatic |
1 | 0 | + | NA | – | NA | GenBank PP964031.1 | |
| 2 | 4 | + | + | + | NA | NA | ||
| 3 | 6 | – | + | + | NA | NA | ||
| 4 | 10 | – | NA | – | NA | NA | ||
| Case 2
Symptomatic |
1 | 0 | + | NA | – | NA | NA | |
| 2 | 4 | – | + | NA | + | NA | ||
| 3 | 6 | – | + | + | NA | NA | ||
| 4 | 10 | – | NA | – | NA | NA | ||
| RT-PCR, reverse transcription followed by polymerase chain reaction; -, negative; +, positive; NA, not available. | ||||||||
**Esta reportagem reflete exclusivamente a opinião do entrevistado.**