Trigeminal neuralgia due to Varicella-zoster virus reactivation
Oliveira DJ et al. - Varicella-zoster virus reactivation
12/08/2024Denise Jourdan Oliveira[1], Diogo Goulart Corrêa[1] and Sérgio Ferreira Alves Júnior[1]
[1]. Universidade Federal Fluminense, Departamento de Radiologia, Niterói, RJ, Brasil.
Corresponding author: Denise Jourdan Oliveira. e-mail: denisejoradio@gmail.com
Authors’ contribution
DJO: study conception, initial drafting of the manuscript, and review of the literature.
DGC: data acquisition and critical revision of the manuscript for intellectual content. SFAJ: data acquisition, analysis and interpretation of data, and critical revision of the manuscript for intellectual content.
All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work.
Conflict of Interest
The authors declare that they have no conflict of interest.
Financial Support
None.
Orcid
Denise Jourdan Oliveira: https://orcid.org/0009-0003-4570-7691
Diogo Goulart Corrêa: https://orcid.org/0000-0003-4902-0021
Sérgio Ferreira Alves Júnior: https://orcid.org/0000-0001-6249-450X
Received 10 April 2024 – Accepted 23 May 2024
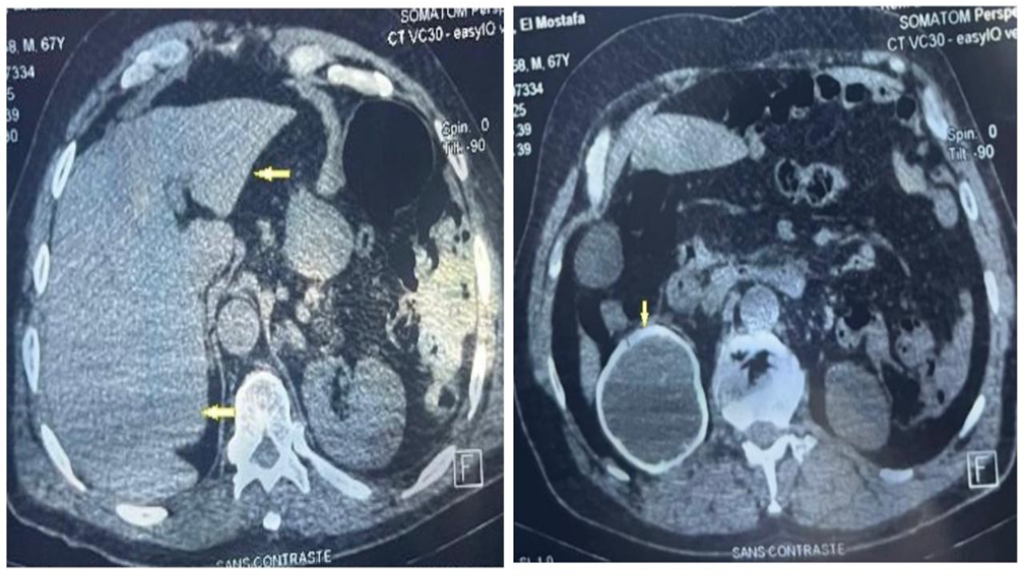
A 61-year-old man presented with left facial pain that worsened with digital touch and was associated with cutaneous vesicles in the left periorbital region for two weeks. Brain magnetic resonance imaging (MRI) revealed a longitudinal lesion with a hyperintense signal on T2-weighted imaging in the left posterolateral portion of the pons and medulla oblongata along the left spinal nucleus of the trigeminal nerve, associated with gadolinium enhancement in the cisternal segment (Figure 1). Cerebrospinal fluid (CSF) analysis revealed mild pleocytosis. Polymerase chain reaction revealed positivity for varicella zoster virus (VZV). Trigeminal postherpetic neuralgia was diagnosed, and the treatment comprised acyclovir, amitriptyline, and gabapentin, which reduced pain intensity and led to the progressive disappearance of the cutaneous lesions.
VZV is a herpesvirus whose primary infection causes varicella (chickenpox). Following primary infection, the virus becomes latent in the sensory neurons of the trigeminal ganglia and/or dorsal root ganglia along the neuraxis1. VZV reactivation is a common complication that occurs spontaneously or in response to several triggers, usually associated with aging and immunosuppression and, in some patients, may cause postherpetic neuralgia2. MRI may demonstrate gadolinium-enhancement of the trigeminal nerve or ganglion due to ganglionitis, and a hyperintense lesion on T2-weighted imaging along the trigeminal nuclei and intra-axial portion, including its entry zone, in patients with postherpetic neuralgia3. The spinal trigeminal nucleus extends from the inferior pons to the medulla and cervical spinal cord and receives sensory information regarding facial pain and temperature4. Thus, its involvement in VZV reactivation may explain the symptoms of postherpetic neuralgia.
References
1 – Niemeyer CS, Harlander-Locke M, Bubak AN, Rzasa-Lynn R, Birlea M. Trigeminal Postherpetic Neuralgia: From Pathophysiology to Treatment. Curr Pain Headache Rep. 2024;28(4):295-306. Available from: https://doi.org/10.1007/s11916-023-01209-z
2 – Skripuletz T, Pars K, Schulte A, Schwenkenbecher P, Yildiz Ö, Ganzenmueller T, et al. Varicella zoster virus infections in neurological patients: a clinical study. BMC Infect Dis. 2018;18(1):238. Available from: https://doi.org/10.1186/s12879-018-3137-2
3 – Cordano C, Caverzasi E, Spigno L, De Maria A, Bandini F. MRI Findings in Varicella Zoster Trigeminal Neuritis Without Rash. Headache. 2018;58(5):764-5. Available from: https://doi.org/10.1111/head.13264
4 – Boeddinghaus R, Whyte A. Imaging of Trigeminal Neuralgia and Other Facial Pain. Neuroimaging Clin N Am. 2021;31(4):485-508. Available from: https://doi.org/10.1016/j.nic.2021.05.008

FIGURE 1: Trigeminal neuralgia due to varicella zoster virus reactivation. Brain MRI demonstrated a longitudinal lesion with hyperintense signal on T2-weighted imaging in the left spinal nucleus of the trigeminal nerve, in the coronal (arrow in A) and axial (arrow in B) planes and on an axial FLAIR (arrow in C), associated with gadolinium enhancement in the cisternal segment of the left trigeminal nerve (arrow in D). PCR of a cerebrospinal fluid sample revealed VZV positivity.