Yakut N– Unveiling Silent Patent Ductus Arteriosus
Nurhayat Yakut[1], Kahraman Yakut[2], Mehmet Gumustas[2], Serap Bas[3] and Ibrahim Cansaran Tanidir[2]
[1]. Basaksehir Cam and Sakura City Hospital, Department of Pediatrics, Division of Pediatric Infectious Diseases, Istanbul, Turkey.
[2]. Basaksehir Cam and Sakura City Hospital, Department of Pediatrics, Division of Pediatric Cardiology, Istanbul, Turkey.
[3]. Basaksehir Cam and Sakura City Hospital, Department of Radiology, Istanbul, Turkey.
Corresponding Author: Dr. Nurhayat Yakut. e-mail: nurhayatyakut@gmail.com
Financial Support: None.
Conflict of Interest: The authors declare no conflicts of interest.
Received 17 February 2025 – Accepted 30 April 2025
Orcid
Nurhayat Yakut: https://orcid.org/0000-0002-6383-0568
Kahraman Yakut: https://orcid.org/0000-0002-9221-5636
Mehmet Gumustas: https://orcid.org/0000-0002-4846-5398
Serap Bas: https://orcid.org/0000-0002-3607-0620
Ibrahim Cansaran Tanidir.: https://orcid.org/0000-0002-1356-0635
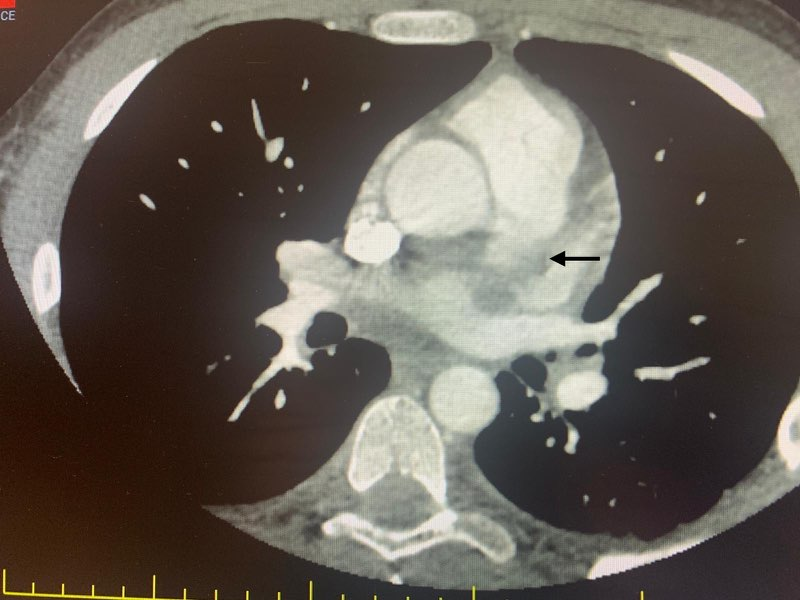
A 16-year-old boy with a previous diagnosis of premature silent patent ductus arteriosus (PDA) was referred to the pediatric infectious disease ward due to COVID-19 pneumonia. Lung auscultation revealed bilateral rhonchi and fine crackles in the lower zones. Initial laboratory tests showed that the absolute lymphocyte count was 700 cells/μL, C-reactive protein level 182 mg/dL, procalcitonin level 6.7 ng/mL, prothrombin time/International Normalized Ratio 1.45, and D-dimer 7.5 μgFEU/mL The patient was started on teicoplanin, ceftriaxone, low-molecular-weight heparin, and aspirin as anticoagulant therapy. Echocardiography revealed hemodynamically significant PDA with thrombosis at the origin of the left pulmonary artery. Anticoagulant therapy was continued. Computed tomography angiography revealed focal thrombus formation near the ostium of the pulmonary artery adjacent to the PDA. A marked tortuosity with aneurysmal changes was seen at the PDA level. A partial thrombus was observed in the pulmonary artery supplying the right lower lobe, and cavitary lesions were observed in the lungs (Figure 1A, B, C). The patient’s clinical condition improved, with fever and cough subsiding. Intravenous antibiotics were continued for four weeks. He was discharged in good clinical condition with ongoing anticoagulant treatment. Three months after discharge, his PDA was closed using a transcatheter method. Although potential complications of clinically silent PDA include infective endarteritis and aneurysmal dilation, there is no consensus regarding routine antibiotic prophylaxis and closure1-3. This case highlights the importance of individualized treatment plans for COVID-19-associated hypercoagulability4 and silent PDA, suggesting that early intervention prevents complications.
Ethical Information: Written informed consent, including the reported images and detailed medical history, was obtained from the patient’s parents for their contributions and permission to publish.
Acknowledgments
None
References
- Gillam-Krakauer M, Mahajan K. Patent Ductus Arteriosus [Updated 2023 Aug 8]. In: StatPearls [Internet]. StatPearls Publish- ing: Treasure Island (FL), 2024.
- Bhat YA, Almesned A, Alqwaee A, Al Akhfash A. Catheter Closure of Clinically Silent Patent Ductus Arteriosus Using the Amplatzer Duct Occluder II-Additional Size: A Single-Center Experience. Cureus. 2021;13(8):e17481.
- Wu P, Zheng C, Zhang F, Wang P, Zhang H, Chen G. Pulmonary artery aneurysm caused by infective endarteritis attributed to patent ductus arteriosus in children: a case report and literature review. Front Pediatr. 2023;11:1181462.
- Conway EM, Mackman N, Warren RQ, Wolberg AS, Mosnier LO, Campbell RA, et al. Understanding COVID-19-associated coagulopathy Nat Rev Immunol. 2022;22(10):639-49.
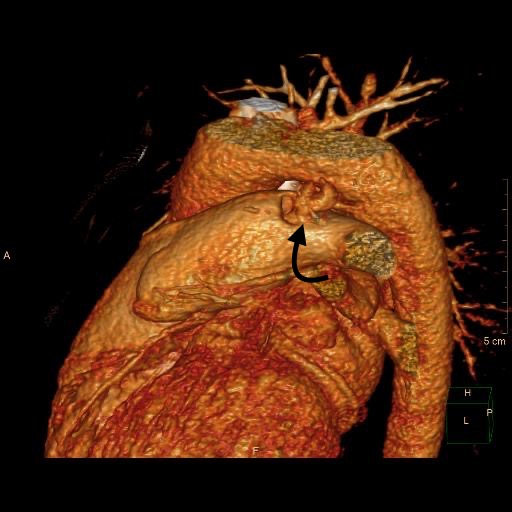
FİGURE 1A: 3D image of the patent ductus arteriosus (PDA).
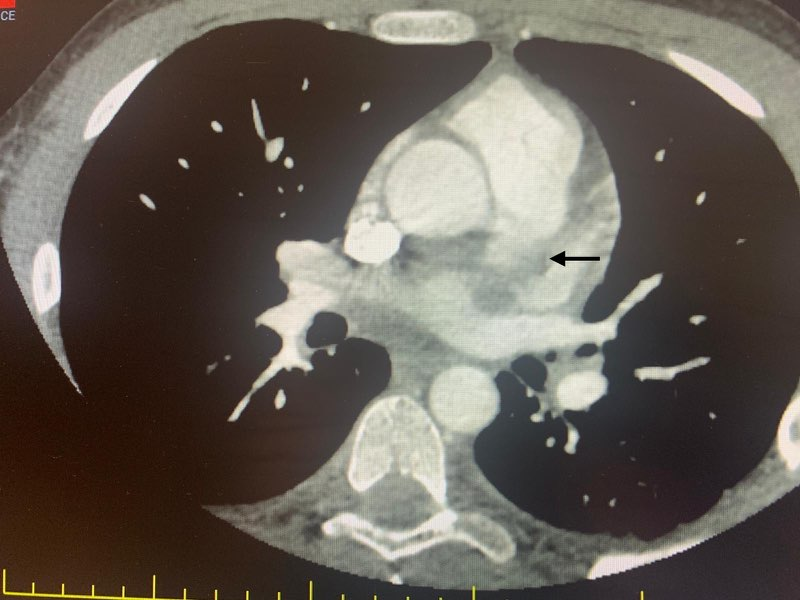
FİGURE 1B: Partial thrombus in the pulmonary artery.

FIGURE 1C: Cavitary lesions associated with septic emboli in the lung.